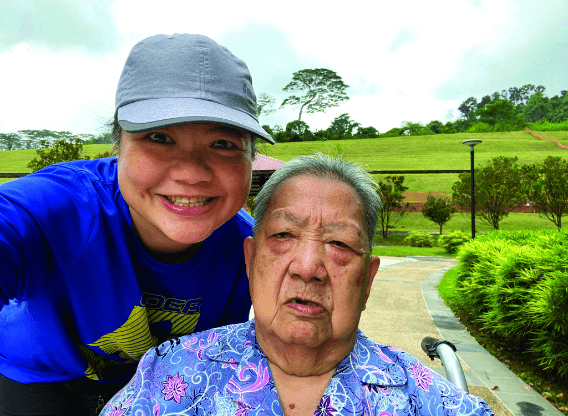
Doing home-based peritoneal dialysis (PD) allows Ms Irene Tam to
have more time to look after her
86-year-old mother.
Ms Irene Tam has been suffering from kidney disease since she was a teenager. In early 2021, she was told
by her doctor that her condition had worsened and her kidneys were failing, and that she required dialysis
to sustain her life.
Irene had two options - peritoneal dialysis (PD), a home-based treatment,
and haemodialysis (HD), in which she would have to visit a dialysis centre thrice a week and spend four
hours each time hooked up to a dialysis machine. For PD, there are two types. One is Automated Peritoneal
Dialysis (APD), where a tube (catheter) is inserted in the abdomen. A special sterile solution enters the
abdomen through the catheter and circulates there, drawing out impurities. The fluid is drained out by a
machine into a bag while the patient sleeps at night, and this procedure is carried out daily. The other is
Continuous Ambulatory Peritoneal Dialysis, which is a machine-free, gravity-based exchange - typically four
to five exchanges per day.
No problem adjusting to PD
The 5I-year-old, who works as a customer service professional, chose the former as it would not affect her
work and earning capacity. It also allows her to have more time to support her 86-year-old mother, who is
bedridden.
To Irene, the APD machine is synonymous with a new loyal “boyfriend” of hers that
accompanies her every night while she undergoes nine hours of dialysis, helping to remove toxins, extra salt
and fluids from her body.
“At the beginning, I was taught how to use the PD machine,” says
Irene. “It’s quite straightforward and not complicated. I also needed to make some adjustments
like how to take care of myself to minimise infection and what I should and should not eat. After
that, no problem.”
To support PD patients like Irene, NKF provides subsidies and has a PD Community Support Programme that
trains patients so that they can carry out the treatment at home on their own, and are clear about
managing risks of infection, proper diet and medication.
The NKF PD nurse makes regular home
visits to Irene’s home to ensure that she is doing well. In this way, knowledge gaps are filled so that
she is empowered to live a quality life.
Irene also joined NKF’s PD Support Group, which helps
equip patients with better health literacy, alleviate psychosocial issues and enable bonding among
patients. “In the group, we share our experiences, encourage and support one another. We have all gone
through similar worries and challenges so we understand each other. It’s therapeutic.”
Happy with her flexible lifestyle
Irene is now doing well in her treatment and rehabilitation and is able to do sporting activities that she loves like playing badminton, cycling, sailing, hiking and bowling. “With PD giving me more flexibility, I’m able to work full-time, take care of my bedridden mother, enjoy outdoor activities and spend time with my friends. I still can have a quality and fulfilling life.”
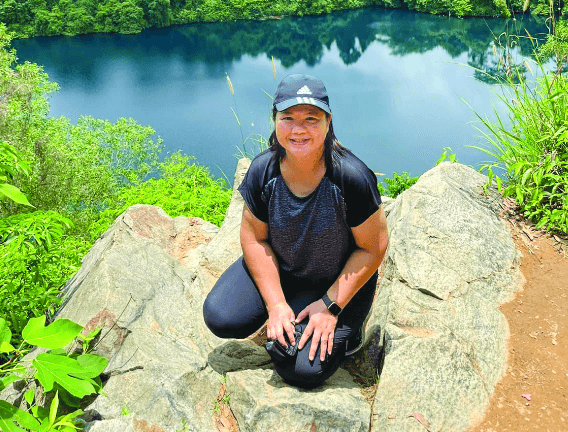
“With PD giving me more flexibility, I’m able to work full-time, take care of my bedridden mother, enjoy outdoor activities and spend time with my friends. I still can have a quality and fulfilling life.”
